Tibialis Posterior Tendinopathy
Adult Flatfoot Reconsteruction
Minimally Invasive Adult Flat Foot Reconstruction
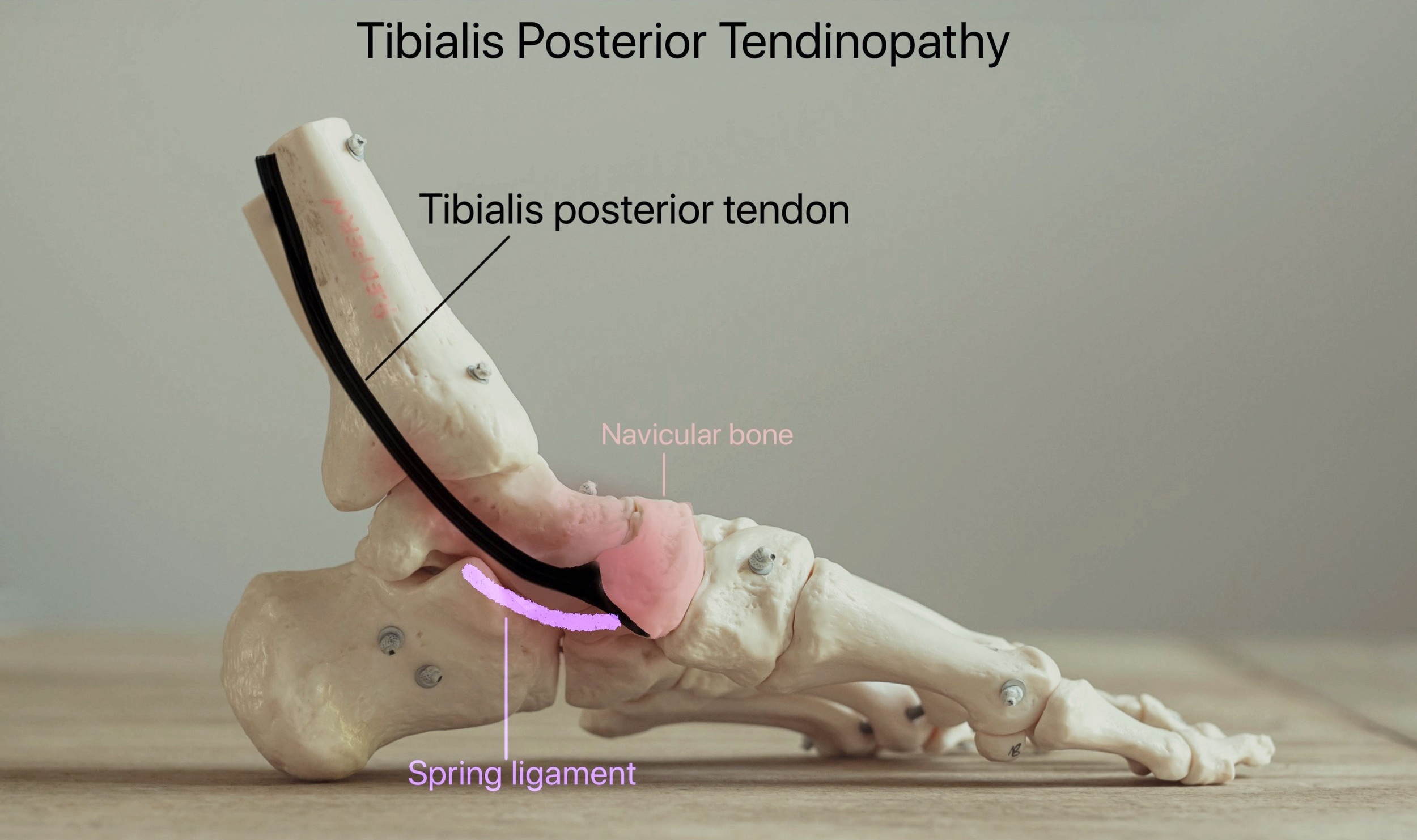
This is a condition in which the foot can become painful and more flat (pes planus). There are several reasons why this can happen but most commonly an important tendon called the Tibialis Posterior is involved, as well as ligaments on the inside of the foot and ankle. Sometimes arthritis can be the cause.
The problem usually, but not always, affects patients who already have a flatter foot shape in the first place.
Adult Aquired Flatfoot Deformity
This photograph shows a severe flatfoot deformity on the left. This required complex reconstructive surgery to both the foot and ankle performed by Mr Redfern.
Reconstructive Surgery
This is a photograph of the same patient after reconstructive surgery by Mr Redfern
As the tibialis posterior tendon becomes weaker and the ligaments become stretched, the foot becomes flatter. As this happens, the heel drifts outwards and the foot itself rolls inwards.
The problem can be complex and may involve structural weaknesses in the ankle, hindfoot and midfoot which need to be carefully identified in order to adequately treat the problem.
Patients usually first notice pain and often swelling on the inside of the ankle area.
The Tibialis posterior tendon can become torn or stretched out. This tendon is important in maintaining the arch of the foot. When it ruptures or becomes stretched out, the arch of the foot becomes flatter and support is lost on the inside of the ankle. This in turn can gradually cause stretch and failure of the supportive ligaments on the inside of the foot which can further worsen the loss of foot shape.
In other patients arthritis can be the primary cause or sometimes an injury can damage the ligaments or tendon leading to gradual failure of these structures. Once torn, the tendon and ligaments will not heal or tighten up again.
Accessory Navicular
Sometimes there is an extra piece of bone on the inside of the foot where the posterior tibialis tendon attaches to the navicular. This is quite common (8% of population). Although most patients do have any symptoms, some may experience pain in the area and may require specialist imaging. In itself it does not cause a flat foot. Surgery may sometimes be required if symptoms persist and generally involves removal or re-attachment of the extra bone.
Treatment
It is most important that an acquired flatfoot deformity is identified at an early stage and that a specialist such as Mr Redfern has the opportunity to assess the foot and arrange specialist imaging such as ultrasound and/or MRI.
Mr Redfern will always recommend non-operative treatment in the first instance if possible. He works closely with podiatrists and physiotherapists and will likely recommend their involvement in your treatment to begin with, along with other recommendations such as a supportive brace to rest the problematic tendon and support the foot structure. Sometimes non-operative measures will be sufficient to control the shape of the foot and avoid pain but surgery is frequently required due to continuing symptoms.
Reconstructive Surgery for Adult Aquired Flatfoot
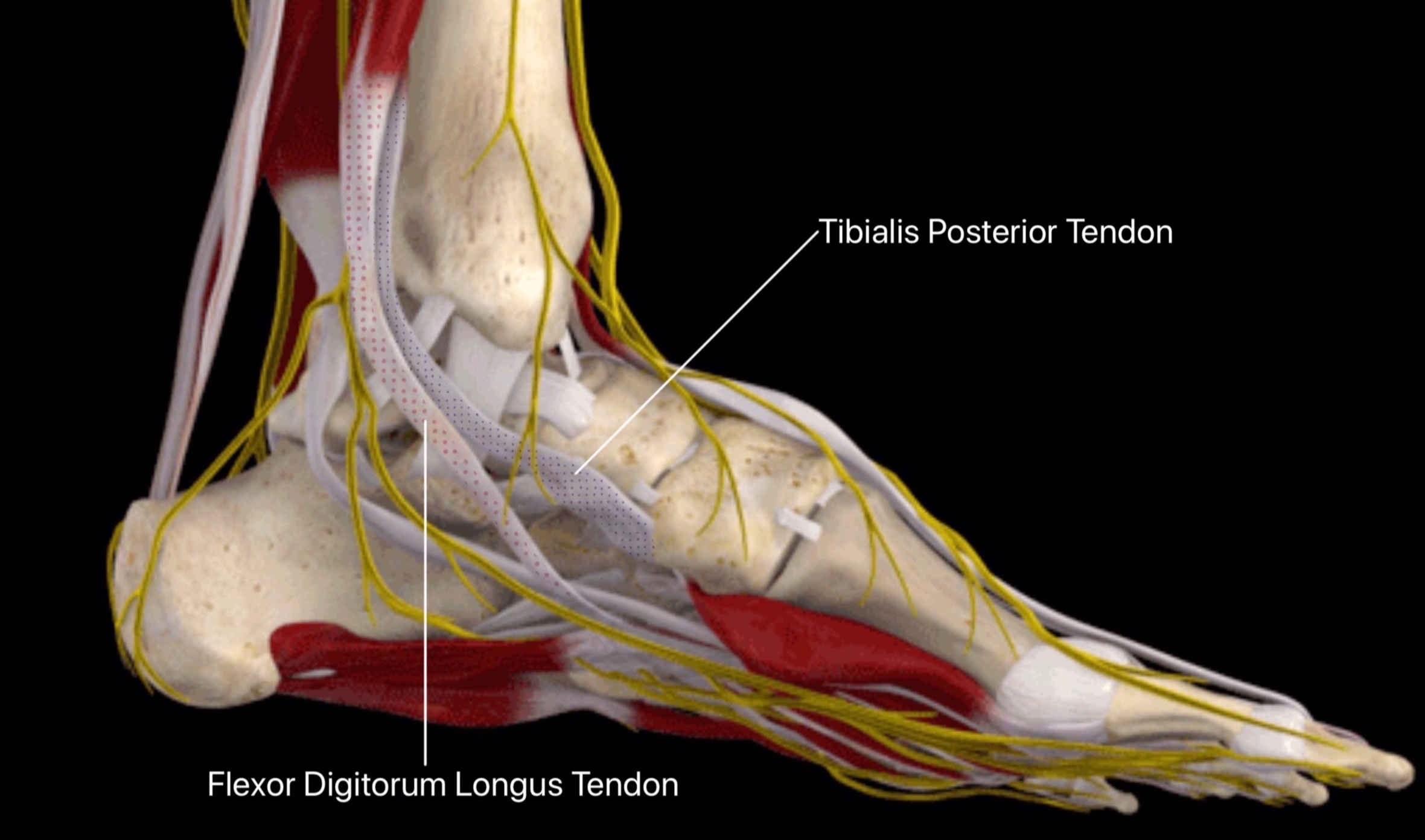
It is not possible to repair the torn tendon, and a new tendon must replace the torn one. The tendon used is one of the many tendons that move the toes and is called the Flexor digitorum longus tendon.
In order to improve the arch of the foot, and protect the tendon transfer something else has to be done to the heel of the foot. A re-alignment of the heel bone (calcaneus) is required by making a cut in this bone (calcaneal osteotomy) and using a screw to fix the bone in a straighter position. Mr Redfern co-developed a keyhole surgery technique to perform this vital element of the surgery through a tiny incision (<1cm) rather than the much larger traditional open incisions which can leave painful/problematic scars or nerve injury. Mr Redfern has taught this new keyhole technique worldwide and several studies have shown it to be a very safe option now. The technique is called MICO (Minimally Invasive Calcaneal Osteotomy)
Sometimes a cylindrical plug is also positioned in the heel joint (subtalar joint) to keep the arch supported and protect the reconstruction (arthroereisis screw).
In other patients the arch is also restored through an additional bone cut in the middle of the foot (Cotton osteotomy) or by fusing joints in the midfoot (eg if arthritis present).
Often patients with an acquired flatfoot also have a bunion / hallux valgus in the same foot and Mr Redfern will often recommend surgical correction this at the same time (usually with keyhole surgery). This too helps to restore the shape and stable structure of the foot.
Post-operative Recovery: General Facts
You will not be walking on the operated leg for 2 - 6 weeks as advised by Mr Redfern
The timing of walking depends on what exactly is done at surgery
In order to stay off your foot, you will need crutches or a walker, and/or a wheelchair.
There will be a hard plaster bandage applied to the leg for two weeks after surgery
Your first follow-up visit will be at approximately 2 weeks to remove the stitches
We will usually apply another cast or boot to wear at this time
If the surgery is on your left ankle, you should be able to drive an automatic vehicle at two weeks. If the surgery is on the right foot, you may drive between at 6 weeks.
Physiotherapy is very helpful to regain the strength and movement of the foot/ankle
You should plan to see a physiotherapist for about at 4-6 weeks as advised by Mr Redfern
There will be moderate swelling of the foot, ankle and leg for about 6-12 months
You can expect to have some soreness and aching for about 4-6 months after surgery
Your strength and movement will continue to improve for about 12-18 months
Main Risks Of Surgery
Swelling - Initially the foot will be swollen and will need elevating. The swelling will disperse over the following weeks and months but will remain evident for up to 6-9 months.
Infection – The risk of deep infection occurring is approximately 1%. You will be given intravenous antibiotics at the time of surgery to help prevent this. It is important to keep the foot elevated over the first 14 days to reduce the swelling and the risk of infection. If there is an infection, it may resolve with a course of antibiotics but could rarely result in failure of the surgery.
Bleeding - Mr Redfern usually performs this surgery under tourniquet (a tight band on the thigh to prevent bleeding) and so there is rarely any significant bleeding at the time of surgery. There can often be some blood seeping into the plaster and bandages after the surgery. This rarely requires more than observation and blood transfusion would be extremely rare (risk <1%).
Delayed or non-union – This is when one of the bone cuts is slow to heal or fails to heal. Up until 6-12 months the lack of bone healing is described as delayed union but if not healed by a year then a non-union is likely. The risk of this is approximately 1%. Smoking increases this risk substantially. If a non-union does occur and it is painful (which is not always the case), then further surgery is usually needed. The chances of the bones not healing properly again after a second surgery is approximately 25%.
Mal-position – Ideally, the surgery is performed so that the bones and tendon transfers heal up in the optimal position for function and appearance. Mr Redfern takes great care to judge the best position during surgery and correct tension for the tendon graft. However, despite his ecperience it is not possible to offer a guarantee of adequate correction and occasionally the foot can become flatter again (risk <5%) although this does not necessarily require any further surgery. If the position is not optimal following surgery, this can usually be accommodated by custom insoles and footwear. Rarely, further surgery may be required.
Nerve damage – There are several nerves crossing the ankle to supply sensation to the ankle and foot as well as controlling muscles in the foot. Despite great care in handling the tissues very delicately, small sensory nerves can be damaged during the surgery and this may leave a patch of numbness in the area of the incision of beyond this. This numbness may be temporary or permanent. There is approximately a 5% risk of this happening. The risk of suffering a nerve injury affecting the muscle function in the foot is <1% in Mr Redfern’s practice.
CRPS - This stands for complex regional pain syndrome. It occurs rarely in severe form and is not properly understood (risk <1% in Mr Redfern’s practice). It is thought to be inflammation of the nerves in the foot and it can also follow an injury. We do not fully understand why it occurs. It causes swelling, sensitivity of the skin, stiffness and pain. It is treatable but in its more severe form can takes many months to recover and can leave persisting pain and sensitivity.
Deep Vein Thrombosis (DVT) - This is a clot of blood in the deep veins of the leg. The risk of a clot occurring is reported as <1% after foot and ankle surgery which is generally substantially lower than after hip or knee surgery. Suspicion of DVT is raised if the leg becomes very swollen and painful. There are tests that can be performed to confirm / exclude the presence of a DVT. If confirmed, you will probably require treatment with a blood thinning agent (heparin preparation and / or warfarin or similar drug such as Rivaroxaban). The main concern with regards a DVT is that rarely (<1:1000 chance with foot and ankle surgery) a piece of clot can break away in the leg and travel to the lungs which is much more serious and can be life-threatening. This is called a pulmonary embolus and signs of this include chest pain and shortness of breath.
Whilst in hospital following surgery it is likely that you will be treated with a blood thinning agent (LMWH - low molecular weight heparin injections) to minimise the risk of DVT/PE but this does not afford total protection and exercises to keep the toes and knee moving are advised, as well as remaining generally mobile. You are also likely be fitted for a compression stocking to be worn on the unoperated leg after surgery.
Once you have left hospital but remain non weight-bearing on the operated leg, you will probably require treatment with a blood thinning agent (low molecular weight heparin injections or oral drugs such as Rivaroxaban or Aspirin). Mr Redfern or his team will discuss this with you whilst you are in hospital.
If you are concerned that the leg has become more swollen and painful (some swelling always occurs after surgery), or if you experience chest pain/shortness of breath, then you should contact Mr Redfern’s team at the hospital, your general practitioner, or the accident and emergency department immediately.
Post-Operative Course: Adult Flatfoot Reconstruction
Day 1
1. Below knee cast (backslab plaster) applied at end of surgery
2. Expect some numbness in foot for 12-24 hours whilst the anaesthetic block is working
3. Pain medication and strict elevation of foot
4. Blood drainage through cast expected and should not cause alarm
Day 2
1. Bathing possible with shower cover (usually provided by ward)
2. Elevation of leg as much as possible for first 2 weeks
3. Mobilisation non-weight bearing with physiotherapist guidance (crutches/frame/scooter)
4. Discharge home usually on day 2–3
5. No weight bearing on the operated leg for the first 6 weeks
2 Weeks
1. Outpatient appointment (OPA) for review of wounds and removal stitches
2. Application of new cast/removable boot at the same appointment
3. If using removable boot then you may remove this to shower/bath if wounds healed
4. You must NOT weight-bear on the operated leg when walking for 6 weeks
5. You may return to driving at this stage ONLY IF left leg surgery and automatic vehicle
(Otherwise you must not drive until 3 months after surgery)
6 Weeks
1. OPA review (cast removed) and allowed to begin weight-bearing in a removable boot
2. No weight bearing without the boot.
3. Boot can be removed at night in bed or when sitting for prolonged periods)
4. To remain in boot until 3 months following surgery
5. Using crutches/frame/scooter until 3 months post surgery
6. Begin physiotherapy (open chain active exercises and gentle passive motion)
12 weeks (3 months)
1. Outpatient review (OPA) with x-ray / scan on arrival
2. Usually the boot can be removed at this stage
3. Continue physiotherapy (closed chain exercises begin) and rehabilitation program
4. Gradually increase activity level as symptoms dictate
5. May return to driving at this stage
6. Still likely to be some swelling and intermittent aching discomfort for 4-6 months
7. Strength continues to improve over 12-18 months after surgery
SICK LEAVE
In general 4 weeks off work is required for sedentary employment, 12 weeks for standing or walking work and 16 weeks for manual / labour intensive work. We will provide a sick certificate for the first 2 weeks; further certificates can be obtained from your GP.
DRIVING
You may return to driving after outpatient review at 2 weeks post surgery only if it was the left leg operated on and only and in an automatic vehicle – otherwise you will be unable to drive until 3 months after surgery.
Typical Milestones
Driving 12/52
Work Depends on occupation, discuss with Mr Redfern
Swimming 12/52 (Hydrotherapy with physiotherapist from 10/52)
Static cycling 10/52
Outdoor Cycling 12/52