MBT Plantar Fasciitis Treatment
The plantar fascia is a thick fibrous band of tissue in the sole of the foot.The term ‘plantar fasciitis’ means inflammation of the plantar fascia. It is this inflammation that causes pain in the heel. Plantar fasciitis is a very common condition.
The plantar fascia is a thick fibrous band of tissue in the sole of the foot. It is attached to the heel bone (calcaneum) and fans out as it passes forwards towards the toes (attaching to the bases of the toes). It helps support the main arch of the foot (behaving a like the string on a bow).
Mr Redfern has developed a methodical approach to treating plantar fasciitis based on treating the underlying mechanical abnormalities and the local heel biology. His keyhole techniques have enabled him to offer state of the art options to these patients.
Plantar Fasciitis
Pain on the undersurface of the heel where the thick supportive tissue attaches (plantar fascia). This picture shows the bone structure of the foot and drawn on top of this is the path of the plantar fascia fanning out from the heel towards the toes. The usual area of pain at the attachment has been shaded under the heel.
Plantar fasciitis may follow a period of prolonged walking or running, often when the person is unaccustomed to such activity. Sometimes it is provoked by poor or inappropriate footwear. The pain is frequently dull and intermittent to begin with and patients often say they tried to ignore the symptoms initially and continue with normal activities. This can aggravate the situation and as time goes on the pain can become sharper and more persistent. The pain is typically worst first thing in the morning and when standing from sitting for a while. Treatment depends upon first confirming the diagnosis and establishing the cause. Mr Redfern will undertake a thorough examination and exclude other causes of heel pain before recommending a treatment regime tailored to the individual.
The problem occurs when part of the inflexible fascia is repeatedly placed under tension, such as during running. It can also occur as a result of unaccustomed exercise.
Repetitive impact causes an overload that produces microscopic tears and inflammation at the point where the fascia is attached to the heel bone.
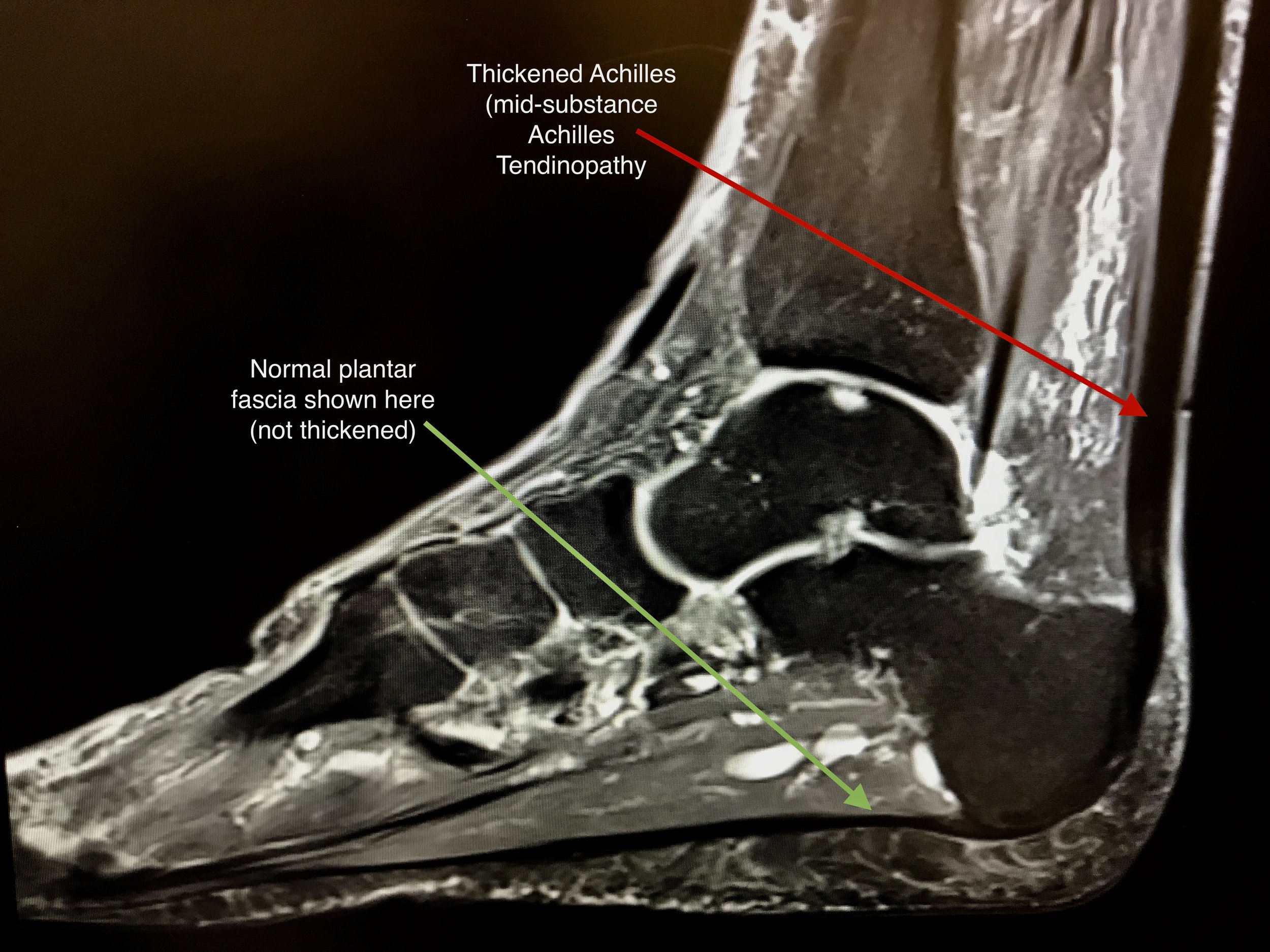
Plantar Fasciitis is a condition which subsides in approximately 90 per cent of affected people spontaneously during a 12 to 18 month period. However, it is difficult to predict how long the condition will last for each individual. The diagnosis can be confirmed with MRI or ultrasound scanning.
Treatment
There are many different treatment options but no actual cure for this condition. Most treatments are therefore aimed at alleviating the symptoms whilst the condition settles with time.
Mr Redfern offers an integrated approach to treatment with a multi-disciplinary team of specialists, including podiatrists and physiotherapists. He will advise the optimal treatment or combination of treatments best suited to each individual patient.
3. Physiotherapy (massage, taping, exercises): This can be a very helpful part of treatment for this condition. Sports physiotherapists will be able to oversee stretching exercises and also offer other treatments such as taping which can sometimes help with the pain.
Mr Redfern will discuss a full range of treatments for plantar fasciitis but here is a basic guide:
1. Activity modification (rest from sport and standing for long periods): Rest and avoidance of sport is very important in trying to tip the scales in favour of repair rather than further injury. Pain should guide and limit the level of activity. Running, racket sports, and long walks are generally best avoided. Cycling and swimming may be less provocative of pain.
2. Calf stretches (to stretch the gastrocnemii): Patients with plantar fasciitis are often tight in their calf muscles. Specifically they tend to be tight in one layer of these muscles called the gastrocnemii. It is very important to undertake stretches to this group of muscles (medial and lateral gastrocnemius muscles) in order to try and decrease stress within the plantar fascia and aid healing of the tissue:
Gastrocnemius Stretches (calf muscle stretches)
Wall Stretch
Begin by standing upright facing a wall over an arm’s length away. Take a large step forward with your uninjured leg and place your hands on to the wall. Now straighten the knee on your injured leg whilst keeping the heel flat on the floor. Then lean your body towards the wall so that you feel a stretch down the back of your calf.
Hold this position for 20 seconds and then relax before repeating.
Hold: 20 seconds
Repeat: 5 times
Frequency: 5 times a day
Stair Stretch
Begin by standing on a small step or the bottom stair of a staircase. Hold on to the bannister or rail to help maintain balance.
Take your injured foot and place it just behind you so that the ball of the foot remains on the step but the heel hangs over the edge of the step. Keeping the knee of your injured side straight, lean your bodyweight through the injured leg and allow the heel to sink below the level of the step as shown in the diagram here. as the heel sinks lower, you will feel the calf muscles stretch in the back of the leg.
Hold this position for 20 seconds and then relax before repeating.
Hold: 20 seconds
Repeat: 5 times
Frequency: 5 times a day
Band stretch
In the seated position, loop a physio ‘theraband’ (specific resistance band) or a towel around ball of foot on the injured side. Gently and steadily pull on the band or towel whilst keeping knee straight. you will feel the stretch in the calf muscles in the back of the leg. Hold the stretch for 20 seconds.
Hold: 20 seconds
Repeat: 5 times
Frequency: 5 times a day
Slant Board
This is something worth considering as it allows you to do stretches easily where and when you want to. The idea is that you stand on the board which has an adjustable pitch which stretches the calf muscles in much the same way as standing on a step but brings the step to you! (see ‘stair stretch’ above). It is particularly useful in an office environment for instance. There are lots of different versions available on the internet. This one is cheap and cheerful and will do the job.
Available at firstaid4sport.co.uk
Extracorporeal Shock Wave Therapy (ESWT)
This is essentially the same technology as lithotripsy which has been used for many years to treat kidney stones
Extracorporeal Shock Wave Therapy (ESWT)
This is essentially the same technology as lithotripsy which has been used for many years to treat kidney stones
5. Ultrasound guided injections (guided corticosteroid injections): If simple measures are not helpful and the pain is severe then ultrasound guided injections of corticosteroid (potent anti-inflammatory) can be helpful. These injections should only be given by a senior doctor under ultrasound guidance. They are given directly to the site of the problem and in the majority of patients will provide at least temporary relief from pain. The duration of relief can be variable but is certainly long term for some patients. If the pain recurs then further injections can be given but no more than 3 injections should generally be given.
6. Anti-inflammatory medication (eg Ibuprofen / Diclofenac): Non-steroidal anti-inflammatory medication can be helpful in treating the pain but are not in themselves curative. Daily “icing” of the painful area can also be helpful. This is sometimes easiest performed by rolling a chilled can of drink (from the fridge not freezer) under the affected foot.
The ESWT is applies to the area of plantar fasciitis on the sole of the foot / heel and encourages the body to heal the tissue as well probably having a direct effect on the nerve endings to desensitise them. The treatment is uncomfortable but very safe. this is an outpatient treatment usually given once a week over a minimum of 3 weeks.
7. Footwear advice (absorbent soled shoes, MBT shoes): A well built, supportive running shoe is often most comfortable but another consideration is a ‘rocker bottom’ style shoe which is available on the high street and online. Flat, thin-soled shoes should be avoided.
8. Orthotics: Inner soles or cushioning heel pads can be bought off the shelf or custom made by a podiatrist and may be helpful.
9. Surgical treatment: In a very small number of cases, Mr Redfern may recommend surgery. Generally this is not considered unless the patient has more than 12 months of persistent pain. Whilst surgery is obviously not a first port of call, there are instances where it can be helpful, especially in patients who have failed previous non-operative treatments.
One operation that he has pioneered in the UK involves removal of painful heel spurs using keyhole surgery under image guidance. Heel spurs can sometimes be responsible for heel pain in conjunction with the plantar fascia. If this is suspected then Mr Redfern will arrange an MRI scan to investigate this and may discuss this state of the art surgery with you.
More commonly, if the calf muscles remain very tight despite diligent stretches then Mr Redfern may recommend a small operation to surgically treat the calf problem. This is performed as a daycare operation and patients are able to walk immediately. Generally, there is very little pain following such surgery and most patients return at 2 weeks after surgery to say that they have hardly used the pain killers (if at all).
10. Other treatments: A whole industry has developed around plantar fasciitis and heel pain. Platelet Rich Plasma is amongst some of the treatments offered by some centres and unfortunately medical research has shown no benefit from this treatment enthuse patients.